Disc herniations are normally a further development of a previously existing disc protrusion, a condition in which the outermost layers of the fibrous ring are still intact, but can bulge when the disc is under pressure. In contrast to a herniation, none of the central portion escapes beyond the outer layers. Most minor herniations heal within several weeks. Anti-inflammatory treatments for pain associated with disc herniation, protrusion, bulge, or disc tear are generally effective. Severe herniations may not heal of their own accord and may require surgery. The condition is widely referred to as a slipped disc, but this term is not medically accurate as the spinal discs are firmly attached between the vertebrae and cannot "slip" out of place.

A SPINAL DISC HERNIATION DEMONSTRATED VIA MRI.
Terminology
Some of the terms commonly used to describe the condition include herniated disc, prolapsed disc, ruptured disc and slipped disc. Other phenomena that are closely related include disc protrusion, pinched nerves, sciatica, disc disease, disc degeneration, degenerative disc disease, and black disc. The popular term slipped disc is a misnomer, as the intervertebral discs are tightly sandwiched between two vertebrae to which they are attached, and cannot actually "slip", or even get out of place. The disc is actually grown together with the adjacent vertebrae and can be squeezed, stretched and twisted, all in small degrees. It can also be torn, ripped, herniated, and degenerated, but it cannot "slip". Some authors consider that the term "slipped disc" is harmful, as it leads to an incorrect idea of what has occurred and thus of the likely outcome. However, during growth, one vertebral body can slip relative to an adjacent vertebral body. This congenital deformity is called spondylolisthesis.
Top of Page
Signs and symptoms
Symptoms of a herniated disc can vary depending on the location of the herniation and the types of soft tissue that become involved. They can range from little or no pain if the disc is the only tissue injured, to severe and unrelenting neck or lower back pain that will radiate into the regions served by affected nerve roots that are irritated or impinged by the herniated material. Often, herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet. Other symptoms may include sensory changes such as numbness, tingling, muscular weakness, paralysis, paresthesia, and affection of reflexes. If the herniated disc is in the lumbar region the patient may also experience sciatica due to irritation of one of the nerve roots of the sciatic nerve. Unlike a pulsating pain or pain that comes and goes, which can be caused by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body. It is possible to have a herniated disc without any pain or noticeable symptoms, depending on its location. If the extruded nucleus pulposus material doesn't press on soft tissues or nerves, it may not cause any symptoms. A small-sample study examining the cervical spine in symptom-free volunteers has found focal disc protrusions in 50% of participants, which suggests that a considerable part of the population can have focal herniated discs in their cervical region that do not cause noticeable symptoms.
A prolapsed disc in the lumbar spine can cause radiating nerve pain. This type of pain is usually felt in the lower extremities or groin area. Radiating nerve pain caused by a prolapsed disc can also cause bowel and bladder incontinence.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the nerves within the spinal column or the cauda equina, both sides of the body may be affected, often with serious consequences. Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. This disorder is called cauda equina syndrome.
Top of page
Cause
Most authors favor degeneration of the intervertebral disc as the major cause of spinal disc herniation and cite trauma as a low cause. Disc degeneration occurs both withdegenerative disc disease and aging. With degeneration the contents of the disc, the nucleus pulposus and anulus fibrosus, are exposed to altered loads. Specifically, the nucleus becomes fibrous and stiff and less able to bear load. The load is transferred to the anulus which, if it fails to bear the increased load, can lead to the development of fissures. If the fissures reach the periphery of the anulus, the nuclear material can pass through as a disc herniation.
Disc herniations can result from general wear and tear, such as when performing jobs that require constant sitting and squatting or driving (sedentary lifestyle). However, herniations often result from jobs that require lifting. Professional athletes, especially those playing contact sports, are prone to disc herniations. Within such an athletic context, it is often the result of sudden blunt impacts against, or abrupt bending or torsional movements of the spinal area. Minor back pain and chronic back tiredness are indicators of general wear and tear that make one susceptible to herniation on the occurrence of a traumatic event, such as bending to pick up a pencil or falling. When the spine is straight, such as in standing or lying down, internal pressure is equalized on all parts of the discs. While sitting or bending to lift, internal pressure on a disc can move from 17 psi (lying down) to over 300 psi (lifting with a rounded back). Herniation of the contents of the disc into the spinal canal often occurs when the anterior side (stomach side) of the disc is compressed while sitting or bending forward, and the contents (nucleus pulposus) get pressed against the tightly stretched and thinned membrane (anulus fibrosus) on the posterior side (back side) of the disc. The combination of membrane thinning from stretching and increased internal pressure (200 to 300 psi) results in the rupture of the confining membrane. The jelly-like contents of the disc then move into the spinal canal, pressing against the spinal nerves, which may produce intense and potentially disabling pain and other symptoms.
Top of page
Pathophysiology
There is now recognition of the importance of “chemical radiculitis” in the generation of back pain. A primary focus of surgery is to remove “pressure” or reduce mechanical compression on a neural element: either the spinal cord, or a nerve root. But it is increasingly recognized that back pain, rather than being solely due to compression, may also be due to chemical inflammation. There is evidence that points to a specific inflammatory mediator of this pain. This inflammatory molecule, called tumor necrosis factor-alpha (TNF), is released not only by the herniated disc, but also in cases of disc tear (annular tear), by facet joints, and in spinal stenosis. In addition to causing pain and inflammation, TNF may also contribute to disc degeneration.
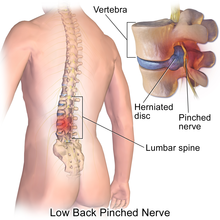
The majority of spinal disc herniation cases occur in lumbar region (95% in L4-L5 or L5-S1). The second most common site is the cervical region (C5-C6, C6-C7). The thoracic region accounts for only 0.15% to 4.0% of cases. Herniations usually occur posterolaterally, where the anulus fibrosus is relatively thin and is not reinforced by the posterior or anterior longitudinal ligament. In the cervical spinal cord, a symptomatic posterolateral herniation between two vertebrae will impinge on the nerve which exits the spinal canal between those two vertebrae on that side. So for example, a right posterolateral herniation of the disc between vertebrae C5 and C6 will impinge on the right C6 spinal nerve. The rest of the spinal cord, however, is oriented differently, so a symptomatic posterolateral herniation between two vertebrae will actually impinge on the nerve exiting at the next intervertebral foramen down. So for example, a herniation of the disc between the L5 and S1 vertebrae will impinge on the S1 spinal nerve, which exits between the S1 and S2 vertebrae.
CERVICAL DISC HERNIATION
Cervical disc herniations occur in the neck, most often between the fifth & sixth (C5/6) and the sixth and seventh (C6/7) cervical vertebral bodies. Symptoms can affect the back of the skull, the neck, shoulder girdle, scapula, arm, and hand. The nerves of the cervical plexus and brachial plexus can be affected. Usually, a posterolateral disc hernia will affect the nerve root exiting at the level of the disk. Nerves roots are numbered according to the vertebral body below them (except the C8 nerve root). Thus, a C5/6 disc hernia will normally affect the C6 nerve root.
LUMBAR DISC HERNIATION
Lumbar disc herniations occur in the lower back, most often between the fourth and fifth lumbar vertebral bodies or between the fifth and the sacrum. Symptoms can affect the lower back, buttocks, thigh, anal/genital region (via the Perineal nerve), and may radiate into the foot and/or toe. The sciatic nerve is the most commonly affected nerve, causing symptoms of sciatica. The femoral nerve can also be affected[29] and cause the patient to experience a numb, tingling feeling throughout one or both legs and even feet or even a burning feeling in the hips and legs. A hernia in the lumbar region often compresses the nerve root exiting at the level below the disk. Thus, a herniation of the L4/5 disc will compress the L5 nerve root.
INTRADURAL DISC HERNIATION
Intradural disc herniation is a rare form of disc herniation with an incidence of 0.2-2.2%. Preoperative imaging can be helpful, but intraoperative findings are required to confirm.[30]
Top of page
Diagnosis
Diagnosis is made by a practitioner based on the history, symptoms, and physical examination. At some point in the evaluation, tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis, degeneration, tumors, metastases and space-occupying lesions, as well as to evaluate the efficacy of potential treatment options.
Physical examination
The straight leg raise may be positive, as this finding has low specificity; however, it has high sensitivity. Thus the finding of a negative SLR sign is important in helping to "rule out" the possibility of a lower lumbar disc herniation. A variation is to lift the leg while the patient is sitting. However, this reduces the sensitivity of the test.
Imaging
- X-ray: Although traditional plain X-rays are limited in their ability to image soft tissues such as discs, muscles, and nerves, they are still used to confirm or exclude other possibilities such as tumors, infections, fractures, etc. In spite of these limitations, X-ray can still play a relatively inexpensive role in confirming the suspicion of the presence of a herniated disc. If a suspicion is thus strengthened, other methods may be used to provide final confirmation.
- Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays. It can show the shape and size of the spinal canal, its contents, and the structures around it, including soft tissues. However, visual confirmation of a disc herniation can be difficult with a CT.
- Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology. It can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors. It shows soft tissues even better than CAT scans. An MRI performed with a high magnetic field strength usually provides the most conclusive evidence for diagnosis of a disc herniation. T2-weighted images allow for clear visualization of protruded disc material in the spinal canal.
- Myelogram: An x-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces. By revealing displacement of the contrast material, it can show the presence of structures that can cause pressure on the spinal cord or nerves, such as herniated discs, tumors, or bone spurs. Because it involves the injection of foreign substances, MRI scans are now preferred for most patients. Myelograms still provide excellent outlines of space-occupying lesions, especially when combined with CT scanning (CT myelography).
- Electromyogram and Nerve conduction studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves, and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury, or whether there is another site of nerve compression. EMG/NCS studies are typically used to pinpoint the sources of nerve dysfunction distal to the spine.
- The presence and severity of myelopathy can be evaluated by means of Transcranial Magnetic Stimulation (TMS), a neurophysiological method that allows the measurement of the time required for a neural impulse to cross the pyramidal tracts, starting from the cerebral cortex and ending at the anterior horn cells of the cervical, thoracic or lumbar spinal cord. This measurement is called Central Conduction Time (CCT). TMS can aid physicians to:
-
- determine whether myelopathy exists
- identify the level of the spinal cord where myelopathy is located. This is especially useful in cases where more that two lesions may be responsible for the clinical symptoms and signs, such as in patients with two or more cervical disc hernias
- follow-up the progression of myelopathy in time, for example before and after cervical spine surgery
- TMS can also help in the differential diagnosis of different causes of pyramidal tract damage.
DIFFERENTIAL DIAGNOSIS
- Mechanical pain
- Discogenic pain
- Myofascial pain
- Spondylosis/spondylolisthesis
- Spinal stenosis
- Abscess
- Hematoma
- Discitis/osteomyelitis
- Mass lesion/malignancy
- Myocardial infarction
- Aortic dissection
Top of page
Prevention
Because there are various causes for back injuries, prevention must be comprehensive. Back injuries are predominant in manual labor so the majority low back pain prevention methods have been applied primarily toward biomechanics Prevention must come from multiple sources such as education, proper body mechanics, and physical fitness.
Education
Education should emphasize not lifting beyond one's capabilities and giving the body a rest after strenuous effort. Over time, poor posture can cause the IVD to tear or become damaged. Striving to maintain proper posture and alignment will aid in preventing disc degradation.
Exercise
Exercises that are used to enhance back strength may also be used to prevent back injuries. Back exercises include the prone press-ups, upper back extension, transverse abdominus bracing, and floor bridges. If pain is present in the back, it can mean that the stabilization muscles of the back are weak and a person needs to train the trunk musculature. Other preventative measures are to lose weight and to not work oneself past fatigue. Signs of fatigue include shaking, poor coordination, muscle burning and loss of the transverse abdominal brace. Heavy lifting should be done with the legs performing the work, and not the back.
Swimming is a common tool used in strength training. The usage of lumbarsacral support belts may restrict movement at the spine and support the back during lifting.
Top of page
Treatment
In the majority of cases, spinal disc herniation doesn't require surgery.
- Initial treatment usually consists of non-steroidal anti-inflammatory pain medication (NSAIDs), but the long-term use of NSAIDs for people with persistent back pain is complicated by their possible cardiovascular and gastrointestinal toxicity.
- Epidural corticosteroid injections provide a slight and questionable short-term improvement in those with sciatica but are of no long term benefit.Complications occur in 0 to 17% of cases when performed on the neck and most are minor.
Lumbar disc herniation
Non-surgical methods of treatment are usually attempted first, leaving surgery as a last resort. Pain medications are often prescribed as the first attempt to alleviate the acute pain and allow the patient to begin exercising and stretching. There are a variety of other non-surgical methods used in attempts to relieve the condition after it has occurred, often in combination with pain killers. They are either considered indicated, contraindicated, relatively contraindicated, or inconclusive based on the safety profile of their risk-benefit ratio and on whether they may or may not help:
Indicated
- Education on proper body mechanics
- Physical therapy, to address mechanical factors, and may include modalities to temporarily relieve pain (i.e. traction, electrical stimulation, massage)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Weight control
- Spinal manipulation: Moderate quality evidence suggests that spinal manipulation is more effective than placebo for the treatment of acute (less than 3 months duration) lumbar disc herniation and acute sciatica.
Contraindicated
Spinal manipulation is contraindicated for disc herniations when there are progressive neurological deficits such as with cauda equina syndrome.
Surgery
Surgery may be useful in those with a herniated disc that is causing significant pain radiating into the leg, significant leg weakness, bladder problems, or loss of bowel control. Discectomy (the partial removal of a disc that is causing leg pain) can provide pain relief sooner than nonsurgical treatments. Discectomy has better outcomes at one year but not at four to ten years. The less invasive microdiscectomy has not been shown to result in a significantly different outcome than regular discectomy with respect to pain. It might however have less risk of infection.
Microdiscectomy (Microdecompression) Spine Surgery
In a microdiscectomy or microdecompression spine surgery, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed to relieve neural impingement and provide more room for the nerve to heal.
A microdiscectomy is typically performed for a herniated lumbar disc and is actually more effective for treating leg pain (also known as radiculopathy) than lower back pain.
Impingement on the nerve root (compression) can cause substantial leg pain. While it may take weeks or months for the nerve root to fully heal and any numbness or weakness to get better, patients normally feel relief from leg pain almost immediately after a microdiscectomy spine surgery.
A microdiscectomy is typically recommended for patients who have:
- Experienced leg pain for at least six weeks
- Not found sufficient pain relief with conservative treatment (such as oral steroids, NSAIDs, and physical therapy).
Microdiscectomy Surgery
A microdiscectomy is performed through a small (1 inch to 1 1/2 inch) incision in the midline of the low back.
- First, the back muscles (erector spinae) are lifted off the bony arch (lamina) of the spine. Since these back muscles run vertically, they can be moved out of the way rather than cut.
- The surgeon is then able to enter the spine by removing a membrane over the nerve roots (ligamentum flavum), and uses either operating glasses (loupes) or an operating microscope to visualize the nerve root.
- Often, a small portion of the inside facet joint is removed both to facilitate access to the nerve root and to relieve pressure over the nerve.
- The nerve root is then gently moved to the side and the disc material is removed from under the nerve root.
Importantly, since almost all of the joints, ligaments and muscles are left intact, a microdiscectomy does not change the mechanical structure of the patient's lower spine (lumbar spine).
LAMINECTOMY SURGERY
A laminectomy is a surgical procedure that removes a portion of the vertebral bone called the lamina. The back muscles are pushed aside rather than cut and the parts of the vertebra adjacent to the lamina are left intact. Recovery occurs within a few days. The surgery is typically performed to alleviate pain from lumbar spinal stenosis. Spinal stenosis is caused by degenerative changes that lead to enlargement of the facet joints in the back of the vertebrae. The enlarged joints and related degenerative changes place pressure on the nerve roots as they exit the spine.
Each vertebra has two portions of vertebral bone over the nerve roots in the back of the spine. These small flat bones are called the lamina.
The lamina functions as a protective covering of the spinal canal. In the lower back, they protect the cauda equina, the nerve roots that branch off of the spinal cord, as well as the nerve roots as they exit the spine.
Removing all or part of the lamina through a lumbar laminectomy can give the affected nerve root more space and a better healing environment.
In a laminectomy surgery:
- The spine is approached through a 2 to 5 inch incision in the midline of the lower back.
- Next, the left and right back muscles, called erector spinae, are dissected off the lamina on both sides and at multiple levels.
- After the spine is approached, the lamina is removed, allowing visualization of the nerve roots.
- The facet joints, which are directly over the nerve roots, may then be undercut, or trimmed, to give the nerve roots more room.
- After the surgeon has confirmed that all pressure has been removed from the nerve, the paraspinal muscles are sewn back together to cover the laminectomy site.
After the lamina and any other sources of pressure on the nerve roots are removed, the nerve roots have room to heal.
Top of page
Epidemiology
Disc herniation can occur in any disc in the spine, but the two most common forms are lumbar disc herniation and cervical disc herniation. The former is the most common, causing lower back pain (lumbago) and often leg pain as well, in which case it is commonly referred to as sciatica. Lumbar disc herniation occurs 15 times more often than cervical (neck) disc herniation, and it is one of the most common causes of lower back pain. The cervical discs are affected 8% of the time and the upper-to-mid-back (thoracic) discs only 1 - 2% of the time.
The following locations have no discs and are therefore exempt from the risk of disc herniation: the upper two cervical intervertebral spaces, the sacrum, and the coccyx. Most disc herniations occur when a person is in their thirties or forties when the nucleus pulposus is still a gelatin-like substance. With age the nucleus pulposus changes ("dries out") and the risk of herniation is greatly reduced. After age 50 or 60, osteoarthritic degeneration (spondylosis) or spinal stenosis are more likely causes of low back pain or leg pain.
- 4.8% males and 2.5% females older than 35 experience sciatica during their lifetime.
- Of all individuals, 60% to 80% experience back pain during their lifetime.
- In 14%, pain lasts more than 2 weeks.
- Generally, males have a slightly higher incidence than females.