
Our surgeons provide the highly personalized and comprehensive orthopedic care for knee replacement surgery. Learn more about knee placement below:
RISKS | PRE-OPERATIVE PREPARATION | TECHNIQUE | PARTIAL KNEE REPLACEMENT | POST-OPERATIVE REHABILITATION |
Knee replacement, or knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability. It is most commonly performed for osteoarthritis, and also for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement.
Other major causes of debilitating pain include meniscus tears, cartilage defects, and ligament tears. Debilitating pain from osteoarthritis is much more common in the elderly.
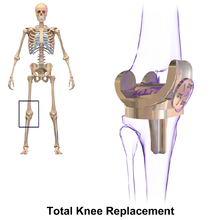
Knee replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
The operation typically involves substantial postoperative pain, and includes vigorous physical rehabilitation. The recovery period may be 6 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility.
|
|
|
|
Knee replacement
Knee replacement surgery is most commonly performed in people with advanced osteoarthritis and should be considered when conservative treatments have been exhausted. Total knee replacement is also an option to correct significant knee joint or bone trauma in young patients. Similarly, total knee replacement can be performed to correct mild valgus or varus deformity. Serious valgus or varus deformity should be corrected by osteotomy. Physical therapy has been shown to improve function and may delay or prevent the need for knee replacement. Pain is often noted when performing physical activities requiring a wide range of motion in the knee joint.
 |
Top of page
RISKS
Risks and complications in knee replacement are similar to those associated with all joint replacements. The most serious complication is infection of the joint, which occurs in <1% of patients. Deep vein thrombosis occurs in up to 15% of patients, and is symptomatic in 2–3%. Nerve injuries occur in 1–2% of patients. Persistent pain or stiffness occurs in 8–23% of patients. Prosthesis failure occurs in approximately 2% of patients at 5 years.
There is increased risk in complications for obese people going through total knee replacement. The morbidly obese should be advised to lose weight before surgery and, if medically eligible, would probably benefit from bariatric surgery.
Fracturing or chipping of the polyethylene platform inserted onto of the tibial component may be a concern. These fragments may become lodged in the knee and create pain or may move into other parts of the body. Recent advancements in production have greatly reduced these issues but over the lifespan of the knee replacement there is potential.
DEEP VEIN THROMBOSIS
According to the American Academy of Orthopedic Surgeons (AAOS), deep vein thrombosis in the leg is "the most common complication of knee replacement surgery... prevention... may include periodic elevation of patient's legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood."
FRACTURES
Periprosthetic fractures are becoming more frequent with the aging patient population and can occur intraoperatively or postoperatively.
LOSS OF MOTION
The knee at times may not recover its normal range of motion (0–135 degrees usually) after total knee replacement. Much of this is dependent on pre-operative function. Most patients can achieve 0–110 degrees, but stiffness of the joint can occur. In some situations, manipulation of the knee under anesthetic is used to reduce post operative stiffness. There are also many implants from manufacturers that are designed to be "high-flex" knees, offering a greater range of motion.
INSTABILITY
In some patients, the kneecap is unrevertable post-surgery and dislocates to the outer side of the knee. This is painful and usually needs to be treated by surgery to realign the kneecap. However this is quite rare.
In the past, there was a considerable risk of the implant components loosening over time as a result of wear. As medical technology has improved however, this risk has fallen considerably. Knee replacement implants can now last up to 20 years.
INFECTION
While it is relatively rare, periprosthetic infection remains one of the most challenging complications of joint arthroplasty. A detailed clinical history and physical remain the most reliable tool to recognize a potential periprosthetic infection.
Top of page
PRE-OPERATIVE PREPARATION
Knee arthroplasty is a major surgery. The xray indication for a knee replacement would be weightbearing xrays of both knees- AP, Lateral, and 30 degrees of flexion. AP and lateral views may not show joint space narrowing, but the 30 degree flexion view is most sensitive for narrowing. If this view, however, does not show narrowing of the knee, then a knee replacement is not indicated. Pre-operative preparation begins immediately following surgical consultation and lasts approximately one month. The patient is to perform range of motion exercises and hip, knee and ankle strengthening as directed daily.
Before the surgery is performed, pre-operative tests are usually done:
- Complete blood count
- Electrolytes
- APTT and PT to measure blood clotting
- Chest X-rays
- ECG
- Blood cross-matching for possible transfusion.
About a month before the surgery, the patient may be prescribed supplemental iron to boost the hemoglobin in their blood system. Accurate X-rays of the affected knee are needed to measure the size of components which will be needed. Medications such as warfarin and aspirin will be stopped some days before surgery to reduce the amount of bleeding. Patients may be admitted on the day of surgery if the pre-op work-up is done in the pre-anesthetic clinic or may come into hospital one or more days before surgery. Some hospitals offer a pre-operative seminar for this surgery.
Top of page
TECHNIQUE
The surgery involves exposure of the front of the knee, with detachment of part of the quadriceps muscle (vastus medialis) from the patella. The patella is displaced to one side of the joint, allowing exposure of the distal end of the femur and the proximal end of the tibia. The ends of these bones are then accurately cut to shape using cutting guides oriented to the long axis of the bones. The cartilages and the anterior cruciate ligamentare removed; the posterior cruciate ligament may also be removed but the tibial and fibular collateral ligaments are preserved. Metal components are then impacted onto the bone or fixed using polymethylmethacrylate (PMMA) cement. Alternative techniques exist that affix the implant without cement. These cement-less techniques may involve osseointegration, including porous metal prostheses.
FEMORAL REPLACEMENT

A round ended implant is used for the femur, mimicking the natural shape of the joint. On the tibia the component is flat, although it sometimes has a stem which goes down inside the bone for further stability. A flattened or slightly dished high density polyethylene surface is then inserted onto the tibial component so that the weight is transferred metal to plastic not metal to metal. During the operation any deformities must be corrected, and the ligaments balanced so that the knee has a good range of movement and is stable and aligned. In some cases the articular surface of the patella is also removed and replaced by a polyethylene button cemented to the posterior surface of the patella. In other cases, the patella is replaced unaltered.
Top of page
PARTIAL KNEE REPLACEMENT
Unicompartmental arthroplasty (UKA), also called partial knee replacement, is an option for some patients. The knee is generally divided into three "compartments": medial (the inside part of the knee), lateral (the outside), and patellofemoral (the joint between the kneecap and the thighbone). Most patients with arthritis severe enough to consider knee replacement have significant wear in two or more of the above compartments and are best treated with total knee replacement. A minority of patients (the exact percentage is hotly debated but is probably between 10 and 30 percent) have wear confined primarily to one compartment, usually the medial, and may be candidates for unicompartmental knee replacement.
Advantages of UKA compared to TKA include smaller incision, easier post-op rehabilitation, better post-operative range of motion, shorter hospital stay, less blood loss, lower risk of infection, stiffness, and blood clots, but a harder revision if necessary. While most recent data suggests that UKA in properly selected patients has survival rates comparable to TKA, most surgeons believe that TKA is the more reliable long term procedure. Persons with infectious or inflammatory arthritis (Rheumatoid, Lupus,Psoriatic ), or marked deformity are not candidates for this procedure.
Top of page
POST-OPERATIVE REHABILITATION
The length of post-operative hospitalization is 5 days on average depending on the health status of the patient and the amount of support available outside the hospital setting.Protected weight bearing on crutches or a walker is required, until the quadriceps muscle has healed and recovered its strength.
Patients typically undergo several weeks of physical therapy and occupational therapy to restore motion, strength, and function. Treatment includes encouraging patients to move early after the surgery. Often range of motion (to the limits of the prosthesis) is recovered over the first two weeks (the earlier the better). At six weeks, patients have usually progressed to full weight bearing with a cane. Complete recovery from the operation involving return to full normal function may take three months, and some patients notice a gradual improvement lasting many months longer than that.
For knee replacement without complications, continuous passive motion (CPM) will can improve recovery. Additionally, CPM is inexpensive, convenient, and assists patients in therapeutic compliance. However, CPM should be used in conjunction with traditional physical therapy. In unusual cases where the person has problem which prevents standard mobilization treatment, then CPM may be useful.
Some physicians and patients may consider having lower limbs venous ultrasonography to screen for deep vein thrombosis after knee replacement. However, this kind of screening should be done only when indicated because to perform it routinely would be unnecessary health care. If a medical condition exists that could cause deep vein thrombosis, a physician can choose to treat patients with cryotherapy and intermittent pneumatic compression as a preventive measure.
Top of page
Contact our office to
Schedule a Knee Replacement Consultation









